The Current Landscape
The global health crisis continues to evolve—not with the urgency of its initial outbreak, but with persistent complexity. The virus hasn’t disappeared; it’s adapted. Today, most regions are no longer in emergency response mode, but ongoing waves of infection remain a real concern. What was once an all-hands-on-deck situation has now become a long-term public health marathon.
Globally, patterns vary. Some countries have successfully integrated COVID-19 management into their public health systems, with stable case numbers and reduced mortality. Others, especially regions facing weaker infrastructure or vaccine hesitancy, still experience periodic spikes. New variants occasionally stir up fresh anxiety, though fewer trigger widespread alarm thanks to improved immunity, vaccines, and treatment options.
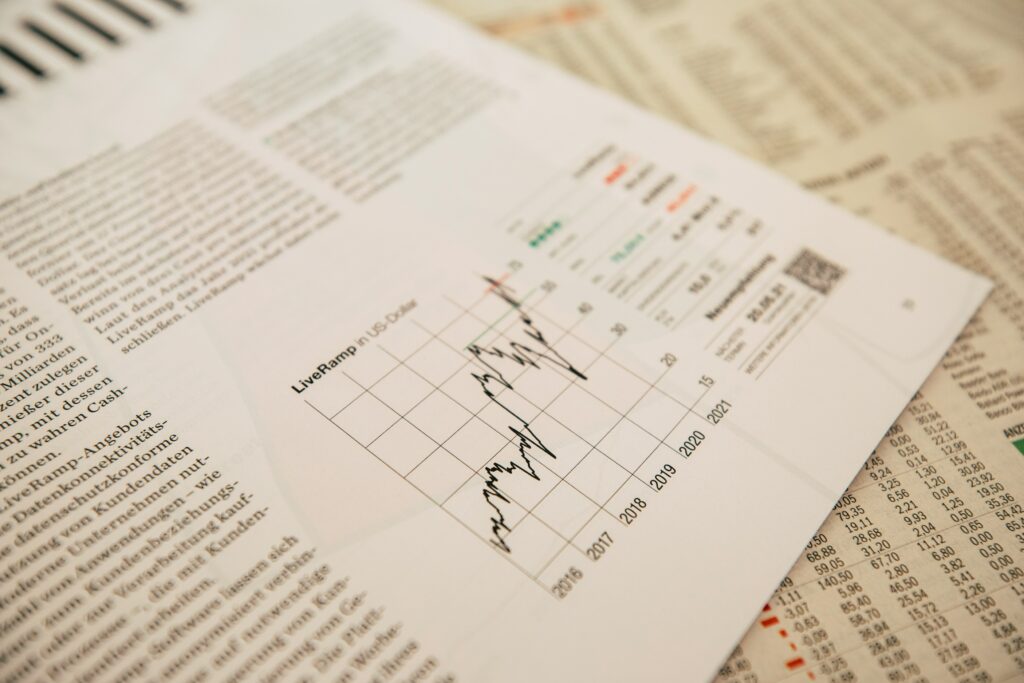
Data shows a pattern of ebb and flow. Case numbers rise seasonally in colder months or after large public events. Hospitalizations and deaths, while lower than peak pandemic levels, still demand attention from health systems—especially as they wrestle with staffing shortages and burnout. This isn’t a crisis in flames, but it still smolders—and for many communities, the risk is far from abstract.
Key Stats That Matter
The numbers keep shifting, but they still tell the story.
Infection rates have stabilized in some areas, dropped in a few, and surged in places with low vaccination or poor adherence to safety protocols. Variants are still in play, and hotspots exist where surveillance is weak. Mortality rates, while lower than peaks from previous years, still trend higher in regions with limited access to care. Recovery rates are improving overall, thanks largely to earlier detection and faster treatment windows.
Vaccination progress is split down the middle. High-income countries continue strong booster campaigns, while low- and middle-income countries lag behind—hampered by supply issues, distribution challenges, or vaccine hesitancy. Access isn’t equal, and that imbalance affects both local containment and global risk.
Hospitals in urban centers are doing better than they were—most have adapted. But rural and under-resourced areas remain stretched. Critical care beds, skilled staff, and oxygen supply are unevenly distributed. A few systems are barely holding the line, while others are catching their breath or starting to rebuild.
Bottom line: the crisis isn’t over, but we’ve come a long way. The data reflects progress—but also ongoing gaps.
Government & Policy Response
Governments are recalibrating—not panicking. Most are steering clear of blanket lockdowns, opting instead for regional, data-driven restrictions. Mandates have become more flexible, dialing up or down based on infection clusters and hospital capacity. Some countries are reintroducing indoor mask rules in transit hubs or high-density areas, while others are ramping up surveillance on new variants at their borders. Overall, it’s less about shutting things down, more about managing complexity in real time.
Travel policies are also more targeted. Full border closures are rare now. Expect testing, proof of vaccination, or digital health passes in place of sweeping bans. Governments have learned that precision beats overreaction—especially for their economies.
Public messaging is getting sharper too. Instead of vague warnings, officials are increasingly leaning on clear metrics and calls to action that are easier to track: get boosted by X date, wear a mask in Y setting, avoid Z behavior in risk zones. The tone has shifted from paternalistic to partnership. For many public health agencies, it’s not about commanding—it’s about convincing.
Medical Advancements & Roadblocks
The vaccine rollout hasn’t slowed—it’s just evolving. Booster shots are getting smarter, with updated formulations tailored to dominant variants. Several mRNA-based vaccines are moving into their next-gen phase, focusing on broader immunity and longer-lasting protection. Trials are also expanding to cover underserved populations and study long-term effectiveness with mix-and-match booster strategies.
Beyond vaccines, the treatment pipeline is heating up. Antiviral drugs, monoclonal antibodies, and even nasal sprays are gaining traction. Some are already in late-stage trials, promising faster recovery and reduced transmission. The most promising development? Treatments that could work across multiple respiratory viruses, not just one.
But while science pushes forward, logistics lag behind. Global supply chains—already bruised from past disruptions—are still struggling to keep up. Shortages in key components like bioreactor bags, cold chain storage, and qualified personnel are slowing distribution in certain regions. Vulnerable countries often sit at the end of the line, and without better coordination, gaps in access could persist long after vaccines and treatments are scientifically ready.
This phase isn’t just about discovery—it’s about delivery, and global systems need to catch up.
Public Behavior & Compliance
The way people respond to health guidelines has shifted—permanently. Early on, there was widespread public compliance, driven by fear, uncertainty, and a sense of shared crisis. Now, that urgency has faded. What’s replaced it is a patchwork of caution, fatigue, skepticism, and selective trust. People still care, but they’re more discerning about who and what they listen to. Blanket mandates no longer move the dial the way they once did.
Trust in health authorities varies greatly—by region, political climate, and past experience. Where transparency and consistency have been strong, adherence to public health guidance remains relatively solid. But in places where institutions have wavered or contradicted themselves, public trust has eroded. That erosion shows up in everything from vaccine hesitancy to resistance around newer precautionary advisories.
As for lifestyle, there’s no going back entirely. Remote work is no longer just a contingency plan—it’s a new baseline. People are traveling differently, with health security and flexibility now top priorities. Personal risk calculations are baked into everyday decisions. The world didn’t hit pause—it rewired. And while the crisis’s acute phase may have passed, its behavioral imprint is here to stay.
Economic Ripple Effects
The health crisis didn’t just overwhelm hospitals—it sent shockwaves through the broader economy. Job markets are still trying to settle. Some sectors, especially frontline services and travel, were gutted and haven’t fully recovered. Others, like logistics, remote tech, and digital healthcare, saw demand skyrocket and stayed hot.
Inflation, meanwhile, isn’t just a line on a graph. It’s hitting wallets across the board—food, fuel, housing. Wages haven’t kept up, and that’s squeezing middle- and low-income households most. In tandem, healthcare systems are carrying a double burden: treating more people with fewer resources, while also absorbing increased operating costs. Staffing shortages haven’t let up. Burnout is driving experienced professionals out of the field.
Some industries—freelance consulting, e-learning, wellness tech—have thrived in the chaos. Others like commercial real estate and traditional retail still look shaky. This is a reshaping, not a rebound.
For a deeper breakdown on where the economy stands now, and what may come next, check out this In-Depth Look at the Economic Impact of Recent Events.
What You Can Do Now
When everything’s in flux, focus on what you can control. Start with the basics: stay on top of personal hygiene. Wash your hands regularly, sanitize shared surfaces, and avoid crowded indoor spaces if you’re feeling off. If masks are recommended in your area, wear one where it counts—especially in high-risk settings.
Next, keep your health data current. That means staying up to date on vaccinations, booster shots, and local health advisories. Stick to reliable sources like government health agencies or established medical institutions. Avoid viral posts with alarmist claims. If the info hasn’t been confirmed by multiple trusted outlets, skip it.
Sign up for notifications from your region’s public health authority. Most now offer real-time updates through text, email, or apps. Set alerts from a news aggregator that pulls multiple reputable sources—don’t rely on one feed to shape your understanding.
Beyond logistics, check in with yourself emotionally. The ongoing nature of the crisis can be draining. Make space for routines that restore you—maybe it’s shutting off the news after a certain hour, or scheduling weekly time to talk with friends. Mental clarity helps with decision-making.
Finally, think ahead. Have a basic plan if things shift suddenly again: a stocked pantry, a go-bag if needed, and a financial safety net if you can manage it. Preparation isn’t panic—it’s smart. This isn’t about living in fear. It’s about staying just one step ahead.
Looking Ahead
Short-term, most public health experts agree: more localized outbreaks are coming. The global picture isn’t uniform—some regions are ramping up response systems, others are barely hanging on. Vaccine fatigue, new variants, and resource shortages are combining into an unstable cocktail. It’s not doom, but it’s not stability either.
We’re also watching a shift from reactive to proactive health planning. Countries are investing—slowly—in digital contact tracing tools, stockpiling essential supplies again, and, in a few cases, training rapid-response teams that can deploy without layers of bureaucracy. The big picture? Governments are trying not to get caught sleeping twice. Whether those systems hold under pressure is a different question.
For individuals and communities, trends suggest more responsibility pushed down to the local level. That could mean keeping up with neighborhood-level alerts, community-led vaccination drives, or school-specific safety protocols. Globally, the markers worth tracking: viral mutation monitoring programs, emergency healthcare readiness scores, and how fast data flows during flare-ups.
Bottom line: the future of crisis preparedness isn’t just about medicine. It’s about streamlined systems, grassroots action, and better communication. No single fix—just smarter tools and faster reflexes.